Taiwan Pediatric Oncology Group (TPOG)-ALL-2013 protocol (TPOG-2013), modifying from St. Jude Total Therapy XV Study and Total Therapy XVI Study, was launched since January 2013. This is the first nationwide minimal residual disease (MRD)-directed protocol for treatment of childhood acute lymphoblastic leukemia (ALL) in Taiwan. According to TPOG-2013, two MRD measurements were scheduled on days 15-19 of induction (MRD1 time point, TP1) and days 35-42, end of induction (MRD2 time point, TP2) to make the definitive risk stratification to guide subsequent therapy.
As of April 30, 2023, 814 newly diagnosed ALLs treated with TPOG-2013 and followed up ≥3 years were enrolled in the study. The outcomes were compared with those of TPOG-ALL-2002 protocol (TPOG-2002) (N=1350, between January 2002 and December 2012), which did not integrate the MRD monitoring. The 5-year event-free survival and overall survival were significantly improved from 76% (95% CI, 74-78) and 81% (80-84) of TPOG-2002 to 86% (83-88) and 89% (87-92) of TPOG-2013, respectively ( P< 0.0001).
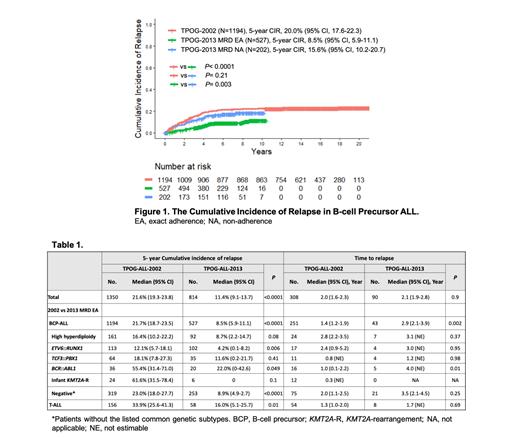
For further analysis of TPOG-2013, 585 (72%) patients with exact adherence (EA) to both TPs were assigned as MRD EA group; 225 patients who were non-adherence (NA) to either one of TPs as MRD NA group; and four patients were excluded for the comparative outcome analysis. For B-cell precursor (BCP) ALL, the 5-year cumulative incidence of relapse (CIR) significantly decreased from TPOG-2002 (N=1194) to TPOG-2013 MRD EA (N=527) ( P <0.0001). However, there was no significant improvement of CIR between TPOG-2002 and MRD NA (N=202) ( P= 0.21) (Figure 1). In MRD EA of BCP-ALL, compared with TPOG-2002, patients with ETV6::RUNX1 or BCR::ABL1 appeared to have significantly lower CIR. Patients without the common genetic subtypes , denoted as “negative” group, also had significant inferior CIR. And the trend of CIR decrease did not attain significant difference in high hyperdiploidy. In contrast, patients with T CF3::PBX1 or infant with KMT2A-rearrangement did not show CIR improvement (Table 1). In T-ALL, compared with TPOG-2002 (N=156), there was a significant decrease of CIR in TPOG-2013 MRD EA (N=58)( P= 0.01)(Table 1), but not in MRD NA (N=23)( P= 0.86).
There was a longer duration to relapse in MRD EA of BCP-ALL. However, a delay of relapse was only demonstrated in patients with BCR::ABL1, which could be addressed by the introduction of MRD-monitoring and TKI inhibitor in TPOG-2013 (Table 1). Further, in term of early relapse before 1.5 year of remission, there was no significant difference in MRD EA of BCP-ALL, compared with TPOG-2002.
In conclusion, this study demonstrated diffident impacts on relapse according to genetic subtypes and MRD adherence. In the negative group of BCP-ALL without the discovery of novel genetic alternations, the relapse could be much decreased with the MRD-directed treatment protocol.
Disclosures
No relevant conflicts of interest to declare.